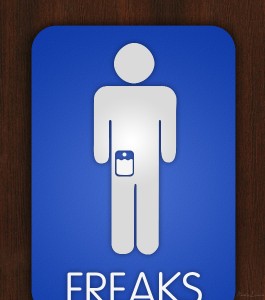
Many people wear their heart on their sleeve, emotions exposed to the world. I wear my bladder on my belly, hidden under shirt and trousers. Some might consider me a freak of nature. I certainly would have thought so not long ago. But, though it would have been news to me then, I’m just one of many hundreds of thousands in the U.S. alone eliminating into an external appliance. Still, despite the numbers, I do find my condition a bit freakish, a violation of some basic design principle—the way people are supposed to be made, existing with a bizarre workaround that reconfigures my plumbing.
About two-thirds of people with a bag stuck to their midsections are living with the aftermath of ileostomies and colostomies, procedures to correct malfunctions of the stomach or colon, with diversions emerging from the small or large intestines to expel digestive waste. I’m one of the remaining one-third with a urostomy, bladderless, urine drained directly from my kidneys to a new body part, an ileal conduit that leads to an external outlet called a stoma.
The Stoma
Of course, that plastic bag doesn’t exist independent of my body. It requires a means of connection to an inner organ. That means is the stoma, a pink protrusion about two inches to the right of my navel. The stoma began life as a piece of my small intestine, five inches of which were removed to fashion the ileal conduit. Urine from my kidneys passes through that conduit and emerges through the stoma into the bag.
The stoma itself, about an inch in radius and an inch high, is fashioned at one end of the reoriented intestine and configured to an opening—as if the tip of another miniature penis has broken through the skin of my midsection to take over the functions of the original. But it has other resemblances, for example, a beef negimaki roll in a Japanese restaurant. In fact, the beef negimaki is pretty much a match in size.
A procedure to be followed every few days involves replacing the collection pouch that goes over the stoma. That means gently removing the old base wafer so that loosening from the adhesive doesn’t harm the skin, cleaning around the stoma with a damp paper towel, cutting an opening the size of the stoma in a new wafer, affixing it over the stoma to the area around it, and finally snapping a new plastic pouch onto the wafer.
That pouch is roughly the size of a real-life bladder dangling from the bulge of my middle. The typical bladder holds about 300-350 ml of urine, the typical pouch about the same, requiring emptying every few hours. Emptying the bag is just a matter of standing over a toilet and opening a release valve. The sound itself replicates normal elimination.
For the great majority of humans with natural bladders the process is much simpler. Males just unzip their flies without worrying about changing bags and maintaining stomas. Females have their own techniques that are apparently more time-consuming, given the lines outside women’s rooms during intermissions. I’m like women in needing the privacy of a stall to unbuckle my belt and drop my trousers. Never again will I be able to use a urinal.
Yet there are several advantages to an external bladder, especially for those of us who are of a certain age. No urgent needs to go when far from a toilet or awakening from pressure several times throughout the night. People like me have the option of a large overnight container that replaces the belly pouch at bedtime and permits hours of uninterrupted sleep.
Still, if I had a choice in the matter, I’d prefer nocturnal trips to the toilet and the internal bladder I was born with. But I didn’t have a choice.
Why No Bladder?
For the great majority of us functioning with urostomy pouches, we got there because of a malignancy, or as some in the medical community call it, bladder C. Among the many interesting bits of information I’ve come across since my diagnosis is the fact that bladder cancer has the highest rate of recurrence of all malignancies, a rate of 80 percent according to one source. The surest way of overcoming that probability is complete bladder removal, not just cutting out the tumor.
Another thing I learned is that a call from your urologist at 10 p.m. is not a delivery of good news. Mine came a week after I left the urine sample during my annual checkup, assuming it was a formality. Analysis discovered microscopic blood particles that indicated a strong possibility of a malignant tumor. The doctor thought he could remove it via a cystoscopy and monitor my bladder with frequent checkups. He did the removal, pulling out a growth the size of a grape. But shortly after that procedure he called again, a bit earlier in the evening, but didn’t sound cheerful. The biopsy revealed the cancer had gotten into the bladder muscle. I’d have several cycles of chemotherapy and surgical removal of the bladder, the prostate, the seminal gland, and some lymph nodes, all to be checked for spreading. The bladder procedure is called a cystectomy, the prostate a prostatectomy.
The bladder, it turns out, consists of three layers—an inner lining, the muscle, and an outer wall. Cancer in the outer wall means a very low rate of survival. But having it in the muscle gave me a seventy percent chance of being around five years after the operation, with three months of pre-surgical chemo adding a few more percentage points.
Web searches and a second opinion verified all that the urologist told me, as did a second opinion. For the chance of living a bit longer I would become a man without a bladder.
Alternatives
Options to an external bladder exist. One is called an Indiana pouch because doctors in that state developed it. It serves as a faux internal bladder but requires emptying through catheterization every few hours. That wasn’t even raised as a possibility for me. Apparently more common is the neobladder, like the Indiana pouch configured from pieces of large and small intestine. Both alternatives extend surgery time by several hours. While the neobladder is also internal, it takes some getting used to, possibly with several months of leakage and incontinence while the user retrains stomach muscles to function like those of the bladder. Doctors advised against the neobladder for someone my age because one study showed a thirty percent failure rate resulting in another more complicated operation to reconfigure for externality.
Although I accepted the medical advice, curiosity led me to search the web for both formal studies and anecdotal patient reports comparing reactions to the internal and external options. In general, despite individual preferences, responses indicated equal satisfaction with either way from the majority of those having cystectomies. Would I be one of the satisfied?
Chemo and Surgery
Perhaps because the impending bladder removal dominated my attention, I never really identified myself as a cancer victim, even during the months of chemotherapy preceding the operation. I leaned back in a padded chair aligned along a wall of a large room with thirty or so other people, tethered to bags that dripped hydration and chemicals into our bodies for hours at a time. From the conversations and from the bald heads of the women with breast cancer, I knew that we all shared malignancies. Yet the room was free of gloom, in part because the oncology nurses were so cheerful and in part because those undergoing the therapy treated the procedure as a minor inconvenience as they chatted with friends, ate meals, and read magazines or screens of iPads and Kindles.
Although, with one exception, I never reacted with nausea, the chemicals really fatigued me, especially one called cisplatin that numbed me into hours of sleep a few days after a treatment. Throughout, I lacked appetite and energy, all for a slightly greater probability of five-year survival. Going for chemotherapy immediately became a natural way of being, another step as I integrated into a new normal.
Perhaps it was just impatience dominating over apprehension, but I was eager for the surgery to be over. Let’s get on with it became my mantra as I counted the days. The sooner I got rid of my bladder the better.
A first step was an appointment with ostomy nurses to introduce me to the functioning of the external pouch and measure my middle for the best spot for the stoma to emerge. That took some logistical manipulation, the ideal spot finally indicated with a black marking pen and covered with clear plastic so that I could shower during the pre-surgery days. My wife was with me, as she was for all of the preparatory sessions, in part to drive and in part to serve as a second memory for the abundance of data we were receiving. For some reason, the process of identifying the stoma spot was amusing, with much laughter in the room. Hysterical on my part?
Surgery itself, on the other hand, wasn’t funny at all. In fact, my preparation began badly when I checked into the hospital the day before and had to clear my bowels by drinking four liters of a liquid called Golytely. Awful stuff, the memory of which still makes me wretch. I couldn’t force down more than half of the container, throwing up at one point and apparently passing out while sitting on the commode, shocking myself to consciousness when my head dropped forward and whacked the wall tiles, smearing them with head wound blood. Though the actual cut was minimal, I sported a large gauze bandage for the next several days, including under the plastic covering I wore in the operating room.
The surgery itself was much easier because I went through it anesthetized, the lingering evidence a scar like a reverse question mark running from my groin to my navel and, of course, the stoma. Post-op pain was minimal, mainly hurting when I burped or had to clear my throat, gestures that pulled at the temporary staples securing the wound. After two days in the ICU, I spent seven more in a hospital room with the goal of passing gas, a sign my innards were functioning.
No one had bothered to warn me about edema. One morning after feeling a pressure between my legs, I lifted my hospital gown to reveal my scrotum swollen to three times its original size. In a great panic I squeezed the call button for the nurse, who when she arrived shrugged and said it was the effect of lymph gland removal. My surgeon just laughed and told me to expect the swelling to last a while and turn the color of an eggplant.
What next? I did have to spend another week in a rehab facility to prove I could dress myself and climb into a bed before being released to go home. Once there, after several visits from a visiting nurse, I signed a release form and am now on my own.
Support
More effective than reading web exchanges has been meeting with the ostomy group at the hospital, mainly because those men and women are survivors who have dealt with external pouches for many years, decades in some cases, leading active lives of work, exercise, travel, all the activity of normal people.
More than three quarters of a million Americans wear external bags. So the ostomy community in the U.S. alone is rather large, but, essentially, we’re a hidden cohort. Other people, the great majority, who function normally, don’t recognize our differences, despite the self-consciousness some newbies feel about their external pouches. For example, it was only after he learned of my diagnosis that a friend discovered a man he had socialized with for ten years had an external bladder. We blend in.
Just recently I learned from the Ostomy Wound Management website a list of politicians and celebrities living and dead who were members of my cohort: “The Queen ‘Mum’ had one – as did Senator Hubert Humphrey, Speaker of the House Thomas ‘Tip’ O’Neill, and actress Loretta Young. Contemporary notables include Rolf Benirschke, Pope John Paul II, actress Barbara Barrie, President George W. Bush’s brother Marvin, and professional golfer Al Geiberger.”
Normal Lives
While I’m still learning about my condition and still healing from the last vestiges of the surgery, a process that can take up to a full year, I’m also assured by others who have gone before me that I’ll return to a life that resembles my old one. Aches and pains will disappear; energy will return; manipulating my pouch will become second nature. In short, though this isn’t the way I came into the world, I’m migrating to a new way of being, different from the mass of men and women, parts I was born with consigned to medical waste, but not quite a freak.